
By Christie R. House
February 2020 | ATLANTA
Patience Zakari, a young mother in rural Nigeria, was afraid to take her children to a clinic when they were sick with fever. She feared the cost of treatment, given her limited budget, which made it difficult to pay for essentials like food and school fees. She preferred, instead, to go to a local chemist to buy cheaper malaria drugs, but they didn’t always work.
When her twins, who were still babies, became ill, she feared they would not survive. She found a clinic operated by the Nigerian United Methodist Church, which was screening for and treating malaria at no cost to the patients. “I, my twins, and my other children all received treatment and are well again. Now that we are receiving free malaria treatment, I no longer fear going to the clinic,” Zakari said.

A strong, integrated health system that families and individuals can trust to give the best care possible is not a given in many parts of the world. In Nigeria, United Methodist health facilities in rural areas are working to improve their outreach into the communities they serve.
The Nigeria Rural Health Program, operated by the Nigeria United Methodist Health Board, oversees 16 rural health clinics in four annual conferences within the Nigeria Episcopal Area. It also supports the newly established Jalingo Hospital, constructed in 2017, thanks to an Imagine No Malaria (INM) Hospital Revitalization Grant.
A Health System Strengthening operational grant from Global Ministries’ Global Health unit supports the operations required to manage the health board’s country office. The grant provides salaries for key program staff, like the health board coordinator, Dr. Godfrey Ogbu. It makes possible supervisory visits and on-the-job training of facility staff at the supported health facilities. This integrated and comprehensive approach to the health needs in Nigeria increases access and improves the quality of services delivered.
A year-long Imagine No Malaria program that began in June 2019 provides long-lasting insecticide bed nets, prophylaxis to prevent malaria, and medications and supplies for diagnosis and treatment. Education encouraging behavioral changes to prevent malaria are included in this outreach to community members.
Reaching patients with services and treatments they need
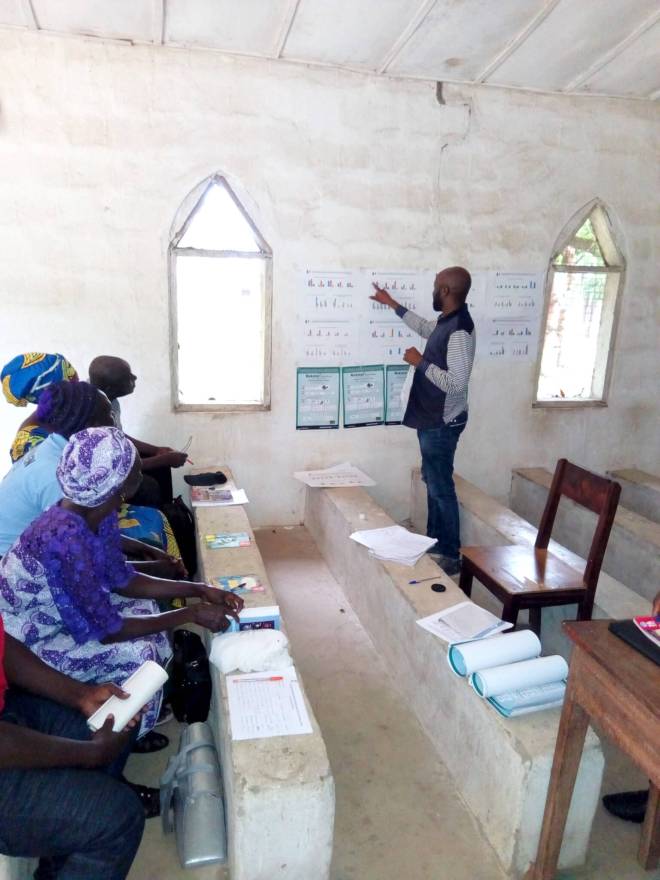
The Nigeria Health Board team travels to United Methodist primary health-care facilities to equip and empower clinic staff with technical information to increase their response. Moses Alikali, who serves as the INM officer in Nigeria, reports that he and Ogbu visited the 16 facilities to monitor malaria programs four times between June and December last year, despite the difficult terrain. Alikali outlines the details involved in one of these visits: “We are making sure that the beneficiaries are receiving free malaria treatment, that health facility staff are adhering to World Health Organization malaria treatment protocol, and that proper documentation of patients and accountability of malaria commodities are recorded.”
Through collaboration with their Maternal, Newborn and Child Health (MNCH) and INM teams, the Nigeria Health Board works toward quality care for all patients who visit the UMC facilities, particularly pregnant women and children under five, who are the most vulnerable to disease. Women who come for prenatal visits can receive medication that will protect them and their babies from contracting malaria. They can also be tested for HIV and if they test positive, start antiretroviral medications. With proper treatment, HIV-positive mothers have a good chance of delivering HIV-free newborns.
This work is vital because Nigeria accounts for 10% of the world’s maternal deaths and ranks 6th in the world for mortality of children under age five. Malaria infection during pregnancy raises risks for both mother and fetus. Maternal anemia, fetal loss, premature delivery and low birth-weight are a few of the dangers.
But the first step is gaining the trust of families so that mothers are aware of their need for the services and come for prenatal visits.
Marta Sunday, who lives near the United Methodist Taka Wurkum facility, found the treatment she needed after she’d tried others: “I was sick for weeks. Even though I was receiving treatment from another health facility, I didn’t recover. At Taka Wurkum, the doctor checked me and explained the reasons why I was still sick. He said either the malaria drugs I bought from the market had expired or I wasn’t taking the right dose. Within two days, the medication he gave me changed everything, and I am feeling good. My baby is calm and healthy since she was treated in this facility. I thank the mission clinic and the doctor in charge who has taken the time to see that these services reach us.”
The Nigeria Health Board also received essential medications and equipment from a HSS Primary Healthcare grant to support gaps in medications and supplies in the targeted health-care clinics. In addition, funds will support the rehabilitation of seven health facilities in Nigeria.
Along with facility revitalization and provision of essential supplies, the HSS program invests in staff development to improve the quality of care. Through a Global Ministries-funded obstetric training event held in the Philippines, a doctor and nurse team received hands-on Caesarian-section training that they brought back to Jalingo Hospital and are sharing with their colleagues.
Working with communities for health improvement
Alikali says community involvement is key for the successful implementation and sustainability of malaria control intervention. “Already in the communities are infrastructures, like community leaders and church leaders, who provide avenues for entry,” he noted.
In its first six months, the INM project directly impacted the lives of 21,075 people, including children, pregnant women, and others. More than 2,038 people who might have died of malaria were saved. The project made quality malaria medications available in hard-to-reach communities. And, the number of patients that visited the health facilities where the INM project has been implemented tripled to 23,991.
The success of this project has boosted the confidence and enthusiasm of the staff in the facilities and the level of community trust as well. This abundant trust has gone a long way to increase health and well-being in remote areas. Receiving correct diagnoses and effective treatments at little or no cost has increased the number of families seeking treatment. The Nigerian Health Board therefore anticipates a general reduction in morbidity in the communities they serve, especially for women and their babies.
Christie R. House is a consulting editor and writer with Global Ministries.

